Tungosis: Symptoms And Treatment
Tungosis is an infection caused by some kind of flea. It mainly attacks the feet. Most of the time, the pathology goes away on its own.

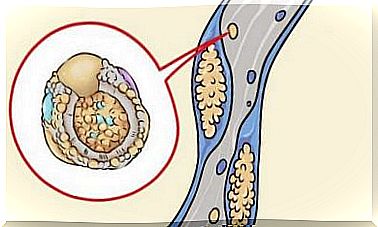
Tungosis is ectoparasitosis, which is a parasitic disease caused by the Tunga penetrans flea. It is an insect smaller than 1 mm in size that penetrates the inside of the skin and causes intense itching, mainly on the feet.
The disease is present in tropical and forest regions of America, Africa and Asia. It is becoming increasingly rare due to the development of villages. The use of shoes and tiled and cement floors prevents their spread.
The chip responsible for the development of tungosis does not have much host specificity. The term host refers to the organism that harbors another within it to establish a symbiotic relationship, that is, for mutual benefit.
In addition to humans, it can affect poultry, dogs and pigs. The habitat where it is most frequently found is dry, sandy, shady and temperate soil. But it is also found in the floors of sheds, barns and animal stables.
Symptoms of tungosis
This disease presents several symptoms. The anatomical area most likely to be infested is the foot. However, the legs, knees, thighs, hands, elbows and other structures of the body have already been affected.
Lesions can be single or multiple, itchy, painful or asymptomatic. The phenomenon of fleas entering the body is asymptomatic. However, after 24 hours, one may start to see an erythematous, itchy macula or papule.
In addition, in the penetration zone, whitish nodules are observed with a central black point corresponding to the abdomen of the flea. Eggs are also often seen attached to the skin near the lesion.
After the flea dies, the lesion is covered with a black scab. This scab is formed by coagulated blood, among other substances, and involuting leaving a scar on the skin.
Although tungosis tends to go away on its own within 4-6 weeks, reinfestation is normal. In addition, the patient usually suffers from other concomitant infections such as:
- Cellulite
- Abscess
- Osteomyelitis
- Thrombophlebitis
- Lymphangitis
- In the most severe cases, sepsis and death
A classification known as the “Fortaleza Classification” was established to standardize clinical descriptions and facilitate recognition of lesions as they progress.
Fortaleza Classification
It is divided into five stages ranging from penetration to involution of the lesion. There are less frequent clinical variants with lesions:
- Crusters
- Pustular
- Ulcerative
- Warts : similar to plantar warts
In step 1, the time elapsed since penetration is 30 to 120 minutes. It is characterized by the appearance of an erythematous macula at the site of penetration.
Stage 2 is 1 to 2 days after infection. In this case, a 1-2 mm macula or hypochromic papule appears with a dark central point (as we have seen, the flea abdomen) surrounded by an erythematous halo.
As for stage 3, it corresponds to the time between 2 and 21 days from penetration. During this time, a whitish, painful papule 3-10mm in diameter with a dark central point appears. There may be hyperkeratosis and a yellowish exudate. Eggs expelled from the flea may be visible.
Continuing with stage 4, a period of time between 3 and 5 weeks, it is worth mentioning the death of the parasite. Subsequently, a halo of necrotic, crusted skin forms around the original lesion.
Finally, at stage 5, which is 6 weeks to several months after penetration, the lesion evolves with the formation of a small epidermal scar which disappears over time.
Treatment
The first step is to remove the intact chip. To do this, the central hole is usually enlarged and the edges are tightened to evacuate the parasite. All of this should be done under aseptic conditions.
Topical antiseptic should be applied to prevent further infections and reduce the risk of complications. Prophylactic treatment against tetanus should also be given.